Muscle builders or physical activity enthusiasts are often confronted with the appearance of injuries or traumas due to poor training or bad posture. Discover in this article the possible micro-traumas.
Pathologies of the tendon
Enthesopathies:
Enthesopathy is a pathology of the tendon. An enthesopathy is a pathology affecting the entheses. The enthesis, from the Greek "enthesis" which means insertion, corresponds to the area of tendino-ligament insertion at the level of the bone. In reality, this pathology concerns the insertion of the tendon but also affects the underlying bone where fatigue fractures can occur.
The pathology can extend to the bursa, which are often interposed between the tendon and the bone in order to facilitate sliding phenomena. Enthesopathies are often related to natural ageing but can be caused by overtraining of the insertion area.
This ageing can manifest itself as intra-tendinous or intra-ligamentary ossification but most often manifests itself as micro-ruptures of the tendon bundles.
Peritendinitis
These are the only real inflammatory lesions. Most often, they are tenosynovitis. They are characterised by the inflammation of a tendon and its synovial sheath. Peritendinitis causes a thickening of the synovial sheath, and is a source of pain when the tendon slides inside it.
Tendonitis Tendonitis, also known as tendinosis, corresponds to a microscopic alteration of the collagen fibres. This alteration causes a disorganisation of these fibres, followed by cellular hyper-density and micro-calcifications. The tendons then form clearly palpable nodules or cysts which are usually located in the middle of the tendon body.
Tendon ruptures
Tendon ruptures are the final stage of tendonitis, although they are relatively rare. Most total ruptures occur in a tendon that has not previously shown any particular signs of pain. Partial ruptures, on the other hand, are a common occurrence in athletes with chronic tendinitis. The most common case is the Achilles tendon rupture.
How is tendonitis diagnosed?
The symptom of tendonitis that prompts the athlete to consult is pain. The questioning of the doctor must then be very precise in order to identify the characteristics of the pathology - whether the pain occurred suddenly (rupture) - the circumstances of the onset of the pain - the timing and frequency of the pain - the consequences on the functional aspect during daily activities; - the consequences on training in terms of duration, intensity and frequency; - the treatments already applied and the respect of a period of relative or total rest. Three signs are necessary to determine tendonitis:
- pain on palpation - pain on palpation
- pain on stretching
- pain on contraction of the same muscle chain involved According to Blazina, tendinopathy can be classified into 4 stages:
First stage: tendon pain occurring after sporting activity and
disappearing easily at rest Second stage: pain at the start of training,
disappearing after warming up and reappearing when tiredness is felt;
Third stage: permanent pain during exercise requiring it to stop or
preventing training.
These pains may intensify, become chronic and persist during daily life; Fourth stage: rupture of the tendon. The clinical examination, as well as the data from the interview, must allow the diagnosis of the tendonitis, to specify the topography of the lesion, and to search for its possible cause.
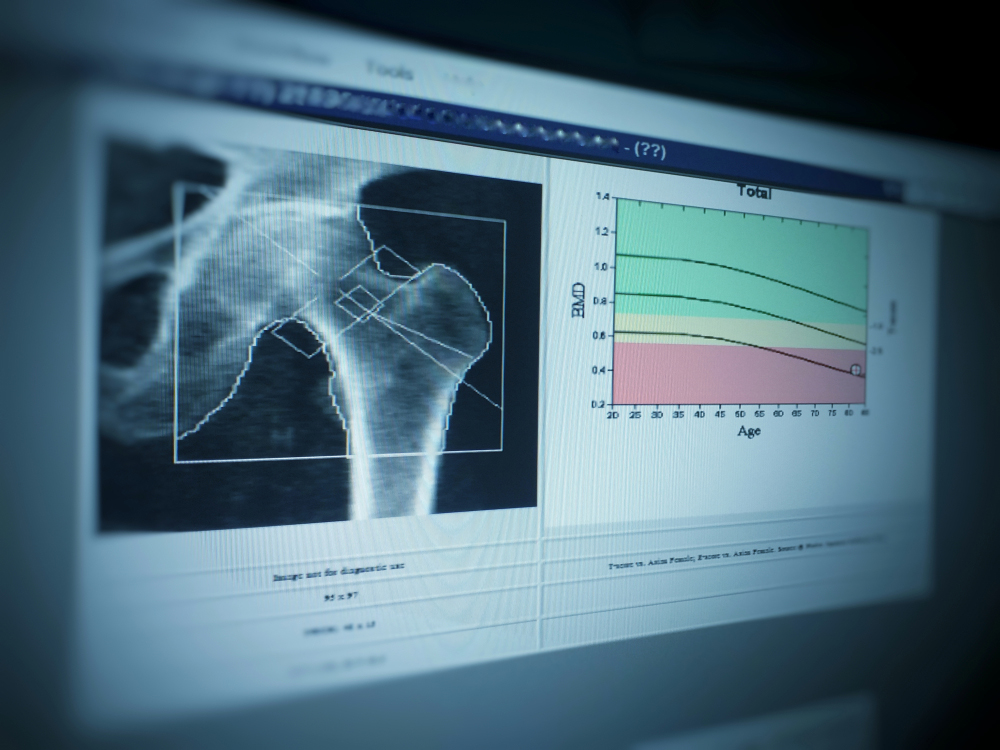
Complementary examinations such as an X-ray, an ultrasound or an MRI only confirm the diagnosis while allowing the existence or not of associated lesions, such as a bursitis, to be specified. Medical treatment is based primarily on rest, combined with massage, stretching exercises and even physiotherapy.
The treatments depend on the location of the tendonitis. The need for surgery, however, is relatively rare.
What is compartment syndrome and how is it treated?
It is a serious condition in which an increase in pressure in a limited space (compartment) significantly disrupts the circulation and function of the musculo-nervous tissues in that space. It occurs mainly in the leg in running athletes, or in the anterior forearm compartment in weight lifters.
Repeated practice can lead to muscle oedema, which can increase the initial muscle volume by 20% to 30%. When the case worsens and reaches the critical point, the muscle is no longer irrigated correctly.
The pain manifests itself in the form of cramps, contractures, or in the form of tension or heaviness of the limb with progressive aggravation. The subject is then obliged to consult a doctor because of the severe pain after the effort. The functional consequences are intermittent claudications leading to a stagnation or even a regression of the level of performance.
The practice of sport and daily life are very limited. The treatment required is generally surgical. It consists of a fasciotomy and must always be performed over the entire height of the compartment and be sufficiently wide to enlarge it.
Micro-trauma to nerves and vessels
Repeated compression of the vascular and neural elements can lead to micro-trauma. These are responsible for localised oedemas, muscular hypertrophy in sportsmen and women who lift loads, or the existence of supernumerary muscles.
The areas most affected are the ulnar nerve (elbow) and the tibial nerve (leg). These lesions affect sportsmen and women who practice exercises that intensively use these areas (throwing, bench press, football, bending). Treatment is usually surgical.
Treatment of training-related micro-trauma
Treatment of the injury is aimed at minimising pain with analgesics and anti-inflammatories with particular emphasis on rest. This does not mean a total cessation of physical activities, but rather ensuring that the athlete does not push himself to the point of pain.
To avoid a recurrence, it is important to identify the factors that caused the injury. Otherwise, a recurrence can occur regardless of the quality of the treatment applied. A better physical preparation and a modification of certain techniques are therefore necessary. Equipment and training may also be questioned.
The steps to take following surgery
Following surgery, the post-operative period consists of 3 periods: The period of healing of the treated lesion; The period of restoration of the locomotor system; The period of resumption of sporting activity. In order to shorten the period of return to sport as much as possible, these three phases can overlap provided that the surgeon, the athlete and the trainer maintain a good dialogue.